How CVS Caremark Puts Patients at Great Risk
Last summer I was diagnosed with Rheumatoid Arthritis. I went to see a rheumatologist after the pain in my hands became so unbearable that I was taking ambien and handfuls of Advil while attempting to uncurl my hands and sleep with them under my stomach. The Advil helped with a bit of the pain, the Ambien allowed me to sleep through worst of it. Sometimes. I was plagued with fatigue and felt depression moving in as my ability to function lessened.
I guess what I’m saying is that RA wasn’t about me feeling achy. It was ruining my life and my family’s life.
Untreated Rheumatoid Arthritis leads to the deterioration of bones, with many sufferers requiring joint replacement surgeries and many more ending up wheelchair bound.
Since August we have tried chemotherapy. It didn’t work. Steriods were useful, but the side effects are very difficult to manage. Simponi offered me relief after just a few months and now that I take it combined with hydroxychloroquine. There are parts of the day where I forget that I have RA. I’m looking forward to having a whole day when nothing hurts.
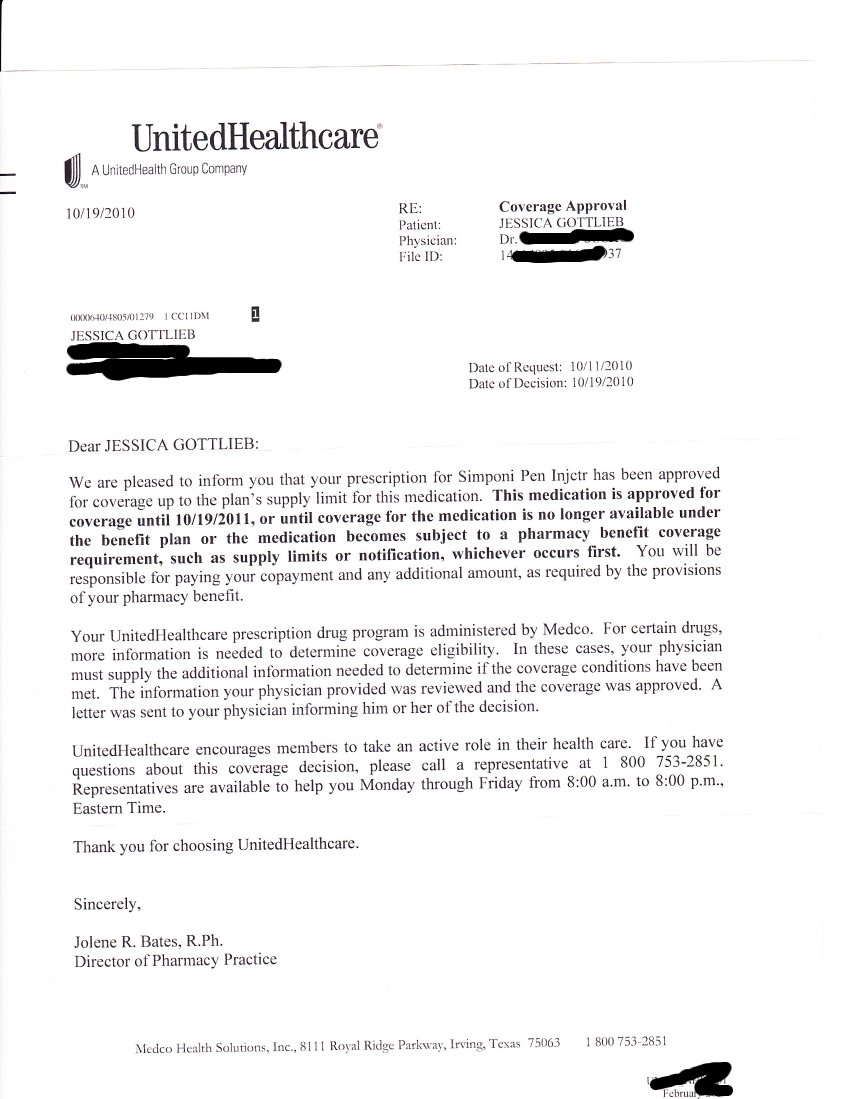
In October of 2010 I received a letter from United Healthcare. It says in part:
We are pleased to inform you that your prescription for Simponi pen Injector [I corrected their spelling on this one] has been approved for coverage…. is approved for coverage until 10/19/2011.
I’m attaching the letter for everyone to see. It is on a United Healthcare Letterhead. Since October I’ve been going to my local pharmacy and picking up my Simponi without issue. Since I hadn’t changed insurance from 2010 to 2011 I had to reason to believe that my prescription status would change. Looking at this letter no one reasonable would believe their coverage expired at the end of the year. On January 20, 2011 I returned to my local pharmacy to get my Simponi. The pharmacist was apologetic. “It’s not covered.” She said.
I stood at the pharmacy blinking back tears. I had a choice to make, my physical well being or my fiscal well being. I chose my physical well being and slapped down a credit card. Simponi costs more than $1,990 for a single dose. I decided that my health was worth nearly two thousand dollars.
To make a very long story short United Healthcare had switched pharmacy providers at the beginning of the year but no prescription cards were ever sent out. No prescription information is listed on UHC health cards. No letters saying “your preapproved prescriptions are no longer valid” were issued. All that was left was me standing at a pharmacy afraid to be sick.
When I got home with my medicine I called United Healthcare and I was advised that the new pharmacy provider was CVS Caremark. Up until January of 2011 I didn’t know that CVS was anything but a retail pharmacy. In my mind it’s the place you go at 2 am when your kids have croup because they’re open 24 hours. CVS is not the place you go on purpose, and it most certainly is not a trusted pharmacy in my neighborhood. The good folks at United Healthcare informed me that I’d have to get my medicine in the mail from CVS.
Really.
Apparently the Simponi pen (which incidentally must be refrigerated) needs to be delivered to my home by the UPS guy. Everyone knows that UPS is much more reliable than a pharmacist.
In addition to the half dozen medications I take to control Rheumatoid Arthritis I have three known serious drug allergies. Each of the medications has a long list of possible side affects as well as a long list of interactions. I’m not popping a tylenol here, this is serious stuff. CVS has given me the terrible choice of a vending machine style pharmacy or poverty.
Moving forward CVS Caremark has graced me with coverage of the Simponi pen for six months, but again only from their mail order pharmacy, and there will be no reimbursement on the pen I had to buy myself in the beginning of the year. Naturally I appealed this decision and the Notice of Action included this paragraph:
Your appeal for reimbursement of Simponi is denied. This medcation requires prior authorization prior to being covered under your prescription benefit plan. Speciality medications must me filled though a Caremark Specialty pharmacy. There are no exceptions regardless of the circumstances.
My experience with Medco was the exact opposite of my experience with CVS Caremark. Medco gave me a year of medicine where CVS gave me six months. CVS Caremark ultimately will cause more paperwork, more doctors visits and more expense for a company who thinks that they are geting a “deal” with them.
I should add that on February 8, 2011 my family received our Prescription Drug Program cards.
CVS caused me to give up two full days of my life to spend on the telephone with them. I won’t even begin to try and tell you who is answering their phones. CVS Caremark is leaving me unreimbursed for two thousand dollars worth of medicine that they know and I know that I need and that I’m entitled to under the plan. CVS has completely dismissed the need for pharmacists and assumed that medical needs can be tended to with shipping labels and telephone trees.
CVS Caremark is attempting to monopolize the supply chain, by providing insurance as well as the delivery of medicine. With CVS Caremark the consumer is left with bad and worse options. Having a pharmacist know what medicines you are taking, and what the possible interactions are is a critical part of healthcare. CVS Caremark has appointed UPS and FedEx as pharmacists and outbound marketers as overseers.
I’m going to pick up the phone and get a mail order pen for this month. I have huge doubts about CVS’s ability to deliver.
I’m going to beg you to please keep this in mind if you’re a benefits manager. I know that Human Resources and Benefits is a very important part of any business. CVS Caremark has so complicated the process of getting proper healthcare your employees will lose time at work if they are forced to deal with CVS Caremark.