Last summer I was diagnosed with Rheumatoid Arthritis. I went to see a rheumatologist after the pain in my hands became so unbearable that I was taking ambien and handfuls of Advil while attempting to uncurl my hands and sleep with them under my stomach. The Advil helped with a bit of the pain, the Ambien allowed me to sleep through worst of it. Sometimes. I was plagued with fatigue and felt depression moving in as my ability to function lessened.
I guess what I’m saying is that RA wasn’t about me feeling achy. It was ruining my life and my family’s life.
Untreated Rheumatoid Arthritis leads to the deterioration of bones, with many sufferers requiring joint replacement surgeries and many more ending up wheelchair bound.
Since August we have tried chemotherapy. It didn’t work. Steriods were useful, but the side effects are very difficult to manage. Simponi offered me relief after just a few months and now that I take it combined with hydroxychloroquine. There are parts of the day where I forget that I have RA. I’m looking forward to having a whole day when nothing hurts.
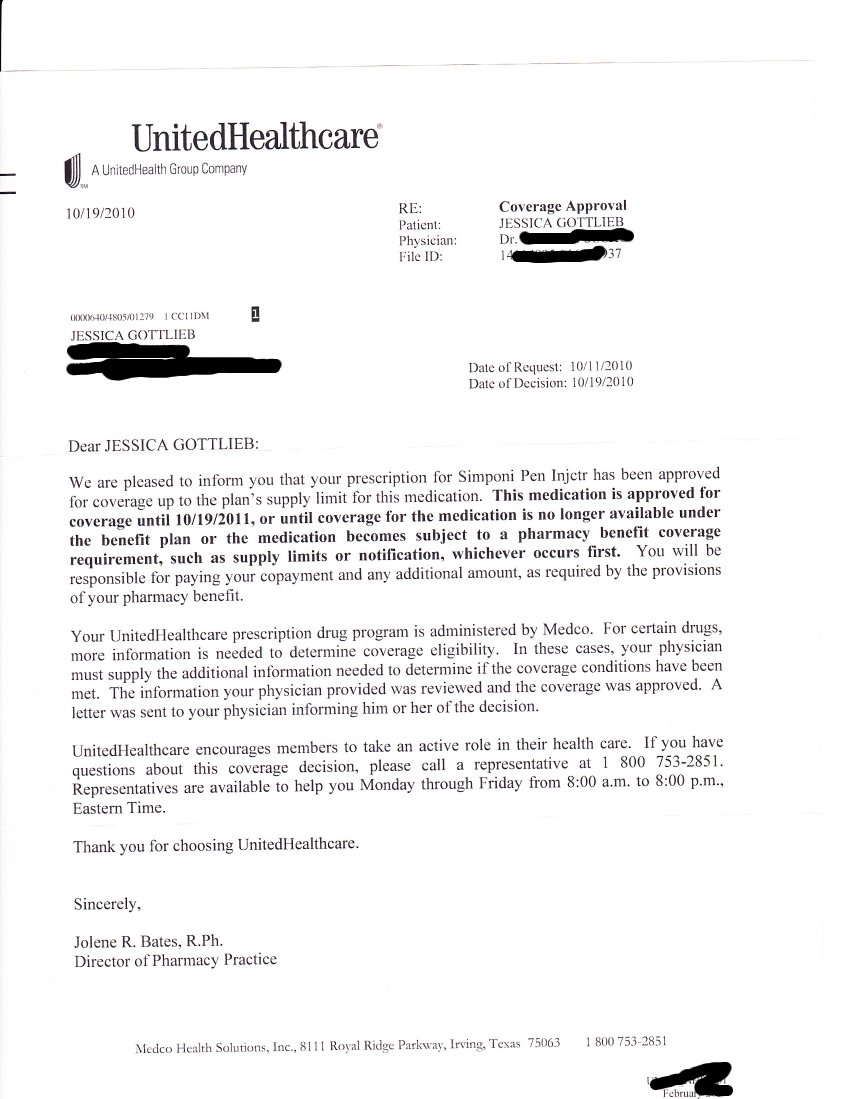
In October of 2010 I received a letter from United Healthcare. It says in part:
We are pleased to inform you that your prescription for Simponi pen Injector [I corrected their spelling on this one] has been approved for coverage…. is approved for coverage until 10/19/2011.
I’m attaching the letter for everyone to see. It is on a United Healthcare Letterhead. Since October I’ve been going to my local pharmacy and picking up my Simponi without issue. Since I hadn’t changed insurance from 2010 to 2011 I had to reason to believe that my prescription status would change. Looking at this letter no one reasonable would believe their coverage expired at the end of the year. On January 20, 2011 I returned to my local pharmacy to get my Simponi. The pharmacist was apologetic. “It’s not covered.” She said.
I stood at the pharmacy blinking back tears. I had a choice to make, my physical well being or my fiscal well being. I chose my physical well being and slapped down a credit card. Simponi costs more than $1,990 for a single dose. I decided that my health was worth nearly two thousand dollars.
To make a very long story short United Healthcare had switched pharmacy providers at the beginning of the year but no prescription cards were ever sent out. No prescription information is listed on UHC health cards. No letters saying “your preapproved prescriptions are no longer valid” were issued. All that was left was me standing at a pharmacy afraid to be sick.
When I got home with my medicine I called United Healthcare and I was advised that the new pharmacy provider was CVS Caremark. Up until January of 2011 I didn’t know that CVS was anything but a retail pharmacy. In my mind it’s the place you go at 2 am when your kids have croup because they’re open 24 hours. CVS is not the place you go on purpose, and it most certainly is not a trusted pharmacy in my neighborhood. The good folks at United Healthcare informed me that I’d have to get my medicine in the mail from CVS.
Really.
Apparently the Simponi pen (which incidentally must be refrigerated) needs to be delivered to my home by the UPS guy. Everyone knows that UPS is much more reliable than a pharmacist.
In addition to the half dozen medications I take to control Rheumatoid Arthritis I have three known serious drug allergies. Each of the medications has a long list of possible side affects as well as a long list of interactions. I’m not popping a tylenol here, this is serious stuff. CVS has given me the terrible choice of a vending machine style pharmacy or poverty.
Moving forward CVS Caremark has graced me with coverage of the Simponi pen for six months, but again only from their mail order pharmacy, and there will be no reimbursement on the pen I had to buy myself in the beginning of the year. Naturally I appealed this decision and the Notice of Action included this paragraph:
Your appeal for reimbursement of Simponi is denied. This medcation requires prior authorization prior to being covered under your prescription benefit plan. Speciality medications must me filled though a Caremark Specialty pharmacy. There are no exceptions regardless of the circumstances.
My experience with Medco was the exact opposite of my experience with CVS Caremark. Medco gave me a year of medicine where CVS gave me six months. CVS Caremark ultimately will cause more paperwork, more doctors visits and more expense for a company who thinks that they are geting a “deal” with them.
I should add that on February 8, 2011 my family received our Prescription Drug Program cards.
CVS caused me to give up two full days of my life to spend on the telephone with them. I won’t even begin to try and tell you who is answering their phones. CVS Caremark is leaving me unreimbursed for two thousand dollars worth of medicine that they know and I know that I need and that I’m entitled to under the plan. CVS has completely dismissed the need for pharmacists and assumed that medical needs can be tended to with shipping labels and telephone trees.
CVS Caremark is attempting to monopolize the supply chain, by providing insurance as well as the delivery of medicine. With CVS Caremark the consumer is left with bad and worse options. Having a pharmacist know what medicines you are taking, and what the possible interactions are is a critical part of healthcare. CVS Caremark has appointed UPS and FedEx as pharmacists and outbound marketers as overseers.
I’m going to pick up the phone and get a mail order pen for this month. I have huge doubts about CVS’s ability to deliver.
I’m going to beg you to please keep this in mind if you’re a benefits manager. I know that Human Resources and Benefits is a very important part of any business. CVS Caremark has so complicated the process of getting proper healthcare your employees will lose time at work if they are forced to deal with CVS Caremark.
Thank you for taking the time to write this story. Visibility of experiences like yours is an essential part of changing the current health care landscape. When I’ve had similar ones, my impulse has been to send a bill to the company to reimburse me for the time/energy I’ve expended. Thanks again for your post.
Jessica, is your health insurance through an employer? If so you should get your HR department involved. UHC most definitely should have let people know about the change to the pharmacy benefit early on. This is especially true for people who have pre-certified medications. Your HR person may also be able to help you get that one month you paid for taken care of. That’s part of what I do at my job (as a Benefits Manager). Unfortunately, we can’t usually control it when an insurance carrier changes pharmaceutical providers. It’s also unfortunate that you are being forced into mail-order if that isn’t right for you. That may be an initiative done by your husband’s company.
We need way more posts like this to bring to light the problems with the current healthcare system. Kudos to you for writing this. Most people have no idea how severely broken the system really is.
There is something really wrong with cvs pharmacy specialists drug I call F B I on them, see if get a billion dollar law suite going out this evil
Empire OUT. And going on every major TV station
I am assuming that the insurance is through your husband’s employer. The majority of group plans are self insured, in which case the employer is paying the claims and not UHC or Caremark (and the employees share in the cost). We have UHC and we do get a pamphlet every year that lists the drug classifications. RA drugs are specialty drugs and most group plans have it set up so that specialty meds are delivered to you to cut out the cost of the retail pharmacy. Specialty med programs are also set up to have a customer care person reach and and contact the insured with any questions. If there is a broker who assists the HR dept that broker is making thousands of dollars in commissions and is there to help the HR person with employee issues. Have them do the legwork for you. They will be able to do the complaining that a letter was not sent out and that you are out of pocket.
P.S. Chances are there is someone who is finding out that their Rx costs and/or circumstances are more favorable now with Caremark than Medco. When a switch is made to a new provider there is always a % of those who are happier and those who are unhappier.
Thank you for this. While I don’t spend near the same amount as you do on meds. I do spend nearly $250 a month (and that is with prescription coverage). I won’t discuss how it took to fight the cinsurance company to approve each of my medications and how much money I paid out until my meds were approved. Something has to be done. These companies just can not decide to stop covering certain meds or determine how a patient can receive the medication. This is a very scarey slippery slope.
Ah, yes. And the Republicans and Tea Party folks will continue to insist that “no one is going to come between me and my doctor” in this, “the greatest healthcare system in the world.” I struggle nearly daily dealing with problems like this pertaining to my child with severe seizures. It’s exhausting and soul-crunching. Take care of yourself —
Exhausting and soul-crunching— I agree. When dealing with my son’s issues years ago and fighting my health insurance company about care that every doctor said he needed, I wanted to put my fist through a wall. Our health care system is broken and criminal. Sending you hugs, Jessica… and you too Elizabeth.
You most definitely should have received paperwork from UHC about the pharmacy change. Typically, we receive paperwork around September regardless of whether or not we plan to change health plans. Open enrollment is in October, which sort of makes it odd that they gave you the letter stating that as if Medco was going to be around come the first of the year.
Have no fear though, before our family had Medco we had Caremark through Blue Cross. I never had a single solitary problem with Caremark.
Jessica, while what CVS is doing isn’t wonderful, the fault truly lies on the shoulders of your health insurance company. THEY made the decision to go with whatever Rx provider was cheapest. They determine the formulary of drugs that will or will not be covered. It is not really CVS’s fault.
United Healthcare does not have a great reputation for being patient advocates. They are, like most health insurance providers, all about their bottom line. As long as theirs is healthy, they don’t care about the actual patient’s well being. And the Universal Healthcare Bill has all of them running scared and disallowing whatever they can before it takes complete effect.
I would be calling UHC and your husband’s HR department about this and leaving CVS for another day.
As much as your praising Medco they are not any better than CVS Caremark or any of the others. Every time I go to the doctor to get medicine to relieve a cold, I constantly have to call the doctors office because Medco refuses to pay for anything but generic. Medco is so cheap they harass my family members about changing their meds to generic because it is cheaper for Medco, but not what the doctor is prescribing. A family member recently ordered meds from Medco directly explaining to them and even faxing over a prescription for Requip? the non-generic form, they sent her the generic pills which is not what she ordered.
I do hope things work out for you.
Did the physician write the prescription with the comment, dispense as written. If not it is the pharmacy’s right to dispense generic. May ask why you are so insistent on branded over generic drugs?
Jessica, I have used CVS sicne they bought up all the local “Mom and Pops” here. I have a medication I need regularly to manage chronic back pain. I just called — this morning– to have my medication transferred. This is absolutely INSANE— THIS is what our healthcare system has become? My hope is that you will continue to fight this through United Healthcare! THEY are the ones to blame as well. Peace on your journey– I know too well how painful it can be!
This seems more to be an issue with your insurance provider, and not an issue with CVS Caremark. Your provider made the choice to go with (what they thought) a cheaper, more cost-efficient prescription service. Our insurance did the same thing about 15 months ago and, while it isn’t fun, it seems to be the wave of the future.
But to blame it on CVS seems wrong…they didn’t make this choice..your insurance company did!
This seems more to be an issue with your insurance provider, and not an issue with CVS Caremark. Your provider made the choice to go with (what they thought) a cheaper, more cost-efficient prescription service. Our insurance did the same thing about 15 months ago and, while it isn’t fun, it seems to be the wave of the future.
But to blame it on CVS seems wrong…they didn’t make this choice..your insurance company did!
I am so sorry you had to go through this Jessica :(
While I know all too well about prior authorizations, it is ridiculous that they are attempting to say you will not be reimbursed for what you were forced to pay. I also think it is nuts how so many people are supposed to rely on “mail-order” pharmacies. My step-sister has MS and was in a fight with MEDCO for a medicine that was necessary for her to be able to function. The poor girl had to beg her father for the money to be able to get her medicine. And with that, the “mail-order” on numerous times wasn’t delivered directly to her but left in her apartment complex’s office, no note on her door, and her not home from class in time to get her meds picked up and refrigerated. While I think I go through hell with my medical, I have no reason to complain when it comes down to situations like this. :(
I think you you are misinformed. The pharmacy does not make decisions on the PA – the formulary and decisions including how long the drug will be approved for are made by your insurance company and not CVS Caremark or Medco. I think if you are writing a blog, you should ask appropriate questions and publish correct information since this can be easily conveyed to you by the pharmacy or your insurance company. The pharmacy facilitate the process of getting the Prior Authorization of the drug, but ultimately your insurance company (United HealthCare) sets the rules.
Retail Pharmacist Consultant
GRH
wrong – CVS does approve/deny PAs as Caremark is the PBM who makes the decisions. CVS is Caremark. I think you should respond and publish correct information when posting comments in blogs.
Hi Jessica. I came across your blog today. I work for the Caremark division of CVS Caremark and I am very surprised you are not being reimbursed for the retail fill. I say this because every prior authorization record has an effective and termination date. My client, Blue Cross, allows me to adjust the effective date to the date of a rejected claim to so the pharmacy can rebill us and reimburse you or you submit a claim to us and we reimburse you directly. Whether UHC allows that would need to be researched. Also, UHC has the option to sign up for Maintenance Choice, which allows patients the choice of picking up their mail order drugs at a CVS or having them home delivered (sort of the whole premise behind the merger of the 2 companies). Again whether UHC elected this benefit would need to be researched, which I would need your approval to do so. Let me know…
If you were truly informed about your prescription coverage as you should be, then you would know that is obviously the result of: 1. faulty commmunication process by UHC, or, 2. You not taking the time to read your open enrollment materials. My guess is it’s the latter if the two. A colossal change in benefits such as this would have been communicated in a timely manner and typically all open refills and PA’s would be transferred. So, my guess is the blame lies on you or your employer’s HR Dept. Maybe you should just appreciate the fact that you have insurance that covers a $2000/mo drug, unlike many others. You really should do your research before you place blame on the messenger.
RPh
I think that your comment embodies all that is wrong with insurance.
How much fine print is the consumer expected to read?
Since when am I supposed to feel “grateful” that my insurance covers medicine I need to function “unlike many others”? To me it sounds like we should all be pissed that everyone doesn’t have access to biologics. FYI medical disability costs everyone a hell of a lot more than $2k/mo
This story is way too familiar to me. I am STILL waiting after a month for cholesterol medication that CVS Caremark claims is lack of cooperation on the part of my doctor. I was in my doctor’s office today and saw the fax with my own eyes that she sent to their Fast Start mail order pharmacy department. As a consumer what recourse do I have? Stop paying my health insurance benefits? All I have left to do is obtain copies and threaten them with a lawyer? It’s absolutely ridiculous. So in the meantime my cholesterol goes untreated, my heart disease gets worse and CVS Caremark meets or exceeds their bottom line? It a few cents less a month for me to get this prescription filled at a CVS pharmacy but my plan dictates that being a “maintenance medication” it must be filled through mail order. It’s good to know that my life is worth CVS Caremark saving a maximum of $12 dollars a year.
cvs care mark does NOT dispense cholesterol medicine… caremark speciality drugs … try cvs retail …know what your talking about
Actually, what you are saying is the exact opposite of true. It of course is sad that you have a condition that requires a specialty medication. But to lie about and slander the employees of Caremark could cause you to get sued. You should be careful about assumptions, they are almost always wrong. The people that answer the phone at CVS Caremark specialty department are all licensed pharmacy technicians, just like the person behind the counter at your pharmacy. There are several pharmacists on staff for each specialty team, and several RNs as well for someone having a medical reaction and not in need of pharmaceutical counseling. The UPS driver puts a box near your door. A box that was packed by, again, licensed pharmacy technicians, under the supervision of Pharmacists, just like your local pharmacy. The only difference? Some of these medications have to be kept at specific temperatures, some have to be handled with special care and while wearing protective equipment or while use flowhoods. The technicians at your local pharmacy? They have no training in these matters and have none of the special equipment. These machines and refrigeration systems cost thousands and hundreds of thousands of dollars. The ability to operate them comes from training and hours of tutorials and safety procedure training, all of which, again, your local pharmacy can not provide their employees. CVS Caremark does provide that and they have some of the best trained staff anywhere. When you call in for your RA drug, you speak specifically to a RA team member. Meaning this licensed technician has taken advance training on RA specific drugs and symptoms. This team member knows as much, if not more, about your medical needs than you do. Since they all took the time and the training to learn about your needs as a patient, you think you might take 5 minutes to learn how their pharmacy operates before lying all over the interenet about them??
“But to lie about and slander the employees of Caremark could cause you to get sued. You should be careful about assumptions, they are almost always wrong. The people that answer the phone at CVS Caremark specialty department are all licensed pharmacy technicians, just like the person behind the counter at your pharmacy.”
1. Those folks answering the phone are a step above the phone bank in India, or maybe a step below, but certainly they are not who I want to talk to. Sue me for saying that idiots answer the phone at insurance companies. That would be fabulous, then everyone who answers the phone for your company would have to take an IQ test to prove I’m liar.
2. I don’t actually use CVS pharmacies because I don’t want to get my medicine from a pharmacy technician. I want to deal with a pharmacist so I’ve sought out smaller stores with one or two pharmacists and one or two techs, that way I can deal with the pharmacist and worry less about errors and bad advice.
Unbelievable that you would threaten and try scare tactics. I know Caremark did not teach you that, so you must have brought that to the table all on your own. Time to find your humanity again. Such a shame. A platform for intelligent, positive feedback in the face of someone’s fear, pain, and frustration and you blew it. No one will hear you now, even if there was a viable point underneath all of that insensitivity.
And on another note, this merger you are complaining about so much because it inconveniences you is very likely a godsend to other employees. When Caremark takes a contract they agree to provide whatever medications are on the formulary that the company hiring them provides. Often, because of the availability of certain specialty meds and the discount Caremark can offer, many before unapproved meds get added to the formulary. Meaning some companies might add in fertility meds for employees trying to conceive, drugs that were not offered before. Also, many companies add on life extending medications for other treatments, like HIV and Hepatitis, because of the savings that Caremark can provide them across the board for all of these medications. So just because you could get your medication at a corner store before does NOT mean that everyone on that insurance plan was able to get their medications at all or conveniently before the change. Once in awhile it is important to look outside yourself at the world around you and not wonder about how this might be inconvenient for you, but instead how it is a blessing for someone else.
I can tell by the way you speak you are probably a fill technician for CVS, and have been drinking the corporate Kool-aid. I have tried Caremark CVS’s mail order for temperature sensitive products and they failed to safeguard the products consecutively, even after I warned them to take precautions, I know I caught it, time to RMA back the trashed product. As for any price savings, my so called 20% share is more than retail at most stores, by more than 10% of retail, this is on a common generic drug, what is CVS Caremark doing price wise to more unique drugs? And if CVS Caremark is so mindful of the public wellbeing, why are they being repeatedly being investigated by the FTC, SEC and members of congress? I think it is time for more investigations like the FDA aimed at CVS Caremark.
Your tone and attitude would be completely different if you walked in her shoes. Shame on you for standing behind a company and not trying to support a person in pain. Could you not have found a way to offer some advice along with some educational company facts? Perhaps you have lost some of your humanity while trudging through your daily grind. I sincerely hope you never feel hopeless at the mercy of a big company and find yourself without the supportive advice and encouragement of strangers.
I think a good number of you are barking up the wrong tree. You need to be mad at your insurance company not the company that gives them discounts on prescription drugs.
At $2000 a shot I would be greatfull to have anybody pay for that. It seems you need a “dose” of reality along with your Simponi.
What “reality” should I be in search of? Having medical insurance leaves people without access to medicine?
You’re not making a whole lot of sense to me.
What a heartless and pointless response you make. Absolutely not helpful!
I’ve used CVS Caremark’s home delivery for over a year for Enbrel and now Simponi. They ship one day and Fed Ex delivers the next. The people who have dealt with me for the most part are very conscientious, pleasant and efficient. I requested that Fed get a signature, after Fed Ex left a shipment in the heat. CVS Caremark gets high marks from me.
Insurance is definitely confusing, especially for people, such as yourself, who do not deal with them on a daily basis. Unfortunately, since you had the medication filled at the retail level, meaning in your local pharmacy, they will not cover it at all. In spite of the company knowing that you need it, as well as you knowing that you need it, they will STILL not cover it just because it was filled at retail level, unless yet another prior authorization is done through them. A prior authorization is when your local pharmacy contacts your doctor, who must then contact your insurance company to see if they will approve the claim. It is a very tedious process, and it is not limited to only CVS/Caremark. Actually all insurance companies require such a thing if a medication is not on their formulary. The prior authorization you receive from your previous insurance provider does not transfer to the company that follows as your coverage. The whole process must be done all over. The company also probably requires it to be filled via mail order since it is a maintenance drug, meaning you will not be coming off of that medication, like you would with say, an antibiotic.
I am also surprised that they would even cover it through mail order. There are plenty of people who NEED medications/procedures done, who have insurance that don’t cover it at all, or there are people who simply don’t have insurance. I’m sure there are people out there who have medications that are more expensive than $2000 per shot. I am not trying to belittle your case, but there is always someone who has it worse out there.
And yes, there are a lot of people who are not familiar with the fact that even though CVS/Pharmacy and CVS/Caremark are both under the same company (CVS), they are two separate entities. So prescriptions are not easily transferable between the two entities. And as another example, a CVS/Pharmacy cannot view your profile/medications filled through Caremark and vice versa. They use two separate systems.
What Bschultz said is absolutely right. Many times you must get it filled through mail order/specialty pharmacy for these types of medications because local pharmacies usually do not have the proper equipment to store such items, nor training, or protective wear.
Igore – yes, there can be mistakes made with the handling of the medication, but everyone is human… even though to you that may not be an excuse. It has nothing to do with drinking “corporate Kool-Aid”. It has to do with understanding the inner workings of local pharmacies, mail order, and specialty pharmacies.
FYI, CVS/Caremark doen not make the rules, they only enforce them. The rules for what is covered and how it is covered is guided by either your employer or health care plan. CVS/Caremark is only the prescription drug manager. Do research before you complain.
Speaking as someone who works at CVS, what Adamwyr says is true. We just fill the prescriptions. Any stipulations or limits come from your insurance provider, which you admitted is United. United is the one giving you 6 months of medication, and United is the one requesting that you use the CVS mail order program. And also, UNITED is the one who won’t reimburse your OOP charges. There’s that old phrase, “Don’t shoot the messenger.” This is exactly what you are doing. Instead of placing the blame with your insurance provider, where it belongs, you have decided to blame the retail pharmacy filling your prescriptions. And, while they might be the easiest target, I suggest you speak to United if you want anything to change.
Be cautious with CVS. They have threatened my son’s health by publishing online. My son worked at CVS in Tampa and was shot twice during a robbery. When CVS would not take care of his needs after being shot I published the issue through a website and was threatened by a corporate CVS attorney that they would become bad people if online publishing didn’t stop. There is true evil in the leadership of that company. My son is still in a wheelchair and in constant pain, unable to work.
Caremark, not off to a good start, somebody needs to be held responsible. The Federal Goverment just changed to using Caremark for mail order pharmacy. Even though I have prescriptions with refills, they are not refilling them timely. Anthem Blue cross is who I pay my premiums to and when you call them for help they have no responsiblity dont you jusl love it. One big RIP OFF. This whole system needs to change and someone needs to be held responsible for this continued abuse of consumers.
I used Caremark for two years for prescriptions for both myself and my wife. I have no complaints. I also have no complaints about the retail CVS pharmacy that we use – for over 5 years – with relationships so strong they know both of our names and ask about our children.
I’m sorry to hear about your problems. I don’t think anyone can make universal claims about companies (good like mine or bad like yours) as we deal with people who can be both professional and helpful (my experience) or unprofessional and uncaring (your experience).
I also have no complaints about my insurance company – who has paid exactly what they promised in their policy, and kept all promises they have made to me over the phone. They also handle any enquiries I have quickly and giving me the benefit of the doubt before another provider or even their own policy.
Again, sorry you don’t have the same experience. I just want to point out that it isn’t that way for me.
I am having the same experience (drug and company).
A useful drug, but unaffordable.
A year later, and I’ve just had the similar misfortune of being switched from Medco to CVS/Caremark. They are doing almost the exact same thing to me for a drug that I take for my MS. Without it, I may no longer be able to drive or even walk up my stairs safely. Medco had given me a prior authorization for it. CVS/Caremark refuses to approve it, no matter how medically necessary nor how much my life will be destroyed without it. It’s like talking to robots. I’ve never dealt with a worse pharmacy “benefit” manager. I am now faced with the prospect of paying $1,000 for a 1-month supply, or having no quality of life. Eat or walk. It’s cruel beyond belief.
By the way, did you hear about CVS/Caremark being accused of using hot blowdryers to take labels off of returned medications, including ones that needed refrigeration, and then repackaging them and selling them again to other unsuspecting customers? Google “CVS/Caremark is evil” and you’ll turn up all kinds of fascinating things.
My heart hurts for you. I’m so sorry. I hope you find a quick resolution and are able to stay well.
Thanks Jessica. Things are still bad. I’ve never dealt with a more callous bunch of people than CVS/Caremark. The last denial letter they sent me was the typographical and written equivalent of screaming in someone’s face. They said that there is no approved medication to treat this particular symptom, and therefore they won’t approve this medication (which has been a godsend in treating this debilitating symptom for the past 2 years). I am now going through some kind of “external” review done by a doctor picked by CVS. It’s a farce.
As for the people saying it’s not CVS that decides what to cover, that’s not exactly true. They have latitude in interpreting what meets the standard for “medically necessary” for a prior authorization. In my case, the drug I’m taking is used very frequently off-label for M.S. Medco approved it as medically necessary once my doctor confirmed why I was using it and that it worked. CVS/Caremark won’t consider it and have turned down every appeal, no matter what evidence, doctor’s letters, research paper etc I’ve sent because it is off-label, and therefore, according to them, not medically necessary by definition, no matter what I nor any of those other things say. A CVS employee coordinating my latest appeal (who just told me yesterday that the latest doctor’s letter and paperwork I’d been told to gather and still in the process of procuring won’t matter because my case has already been forwarded on without anyone having told her) told me on the phone that CVS/Caremark interprets the definition of “FDA approved” differently from Medco.
This is crazy making.
That in and of itself should be approval. You have MS not insomnia. It’s like people stop being human when they make these policies.
I have had nothing but trouble from the Caremark Specialty Pharmacy since my insurance switched to them in January. Like other commenters, Caremark insists the only delay in starting medications is that they have not received communications from my doctor despite the doctor’s office being able to produce a paper trail for me that clearly proves the opposite (read: Caremark is lying). I can only hope for the best, but I don’t think I will get it.
I’m switching to CVS/Caremark due to my company’s insurance company so I was just checking how reliable they are, not like I have much choice, but just to be ready to whatever comes at me.
Tried to scan anything that would invalidate the blogger’s argument, but most of the negative replies I see are either nonsensical, or lack of knowledge of the poster of the situation, maybe not in the general pharmacy sense but not the situation.
For example, to the person saying that they worked at CVS, why are you telling the blogger to complain to United? United doesn’t handle prescription insurances anymore. At least in my case the subscribers got transferred to Caremark/CVS _which_ is an insurance provider.
And you know that the ‘best trained staff’ stuff is a gimmick right?
I worked at two companies.
First one’s training lame, employee well being sucks.
Second one’s training nonexistent, employee well being good.
Though I don’t have to deal much with customers much though so it might be different.
Gee maybe you should do YOUR homework since CVS Caremark dispenses Zetia 10mg 90 tablets to me every 3 months with instructions on the bottle that reads ~AND I QUOTE”take 1 tablet daily for treatment of cholesterol”.
Do you have any advice for a friend of mine…her father has this insurance (CVS Caremark) and they have denied his chemo. He has a fast-growing type of brain cancer and they are extremely afraid and angry trying to fight the insurance company. The oncologist is working hard on their behalf as well. Is there a contact person or advocacy group my friend could contact?
I would call my local news stations. All of them.
I’d try my best to use the media and treat it as the life and death situation it is.
I’m really sorry you’re being forced to do this.
You need to contact your insurance company not caremark
I just had a similar experience with CVS CARENOT. Late July 2012: They required a pre-auth which my Dr faxed to them, then LIED to me on the phone Aug 14th stating my Drs office HAD NOT sent anything in & there was NO PENDING ACTION or DENIELS in process for this specific pre-auth. Came to find it had been DENIED because………….. drum roll………… there was an existing pre-auth in place thru 3/2013 !!!! So, I was without the med for 2 weeks…….the $$ they avoided were not a lot, but multiply this times the number of people they’re doing this to & it’s BIG BUCKS. These lying scum need to be taken down !!! Oh, & this is just a generic drug………..
CVS Caremark screwed me over also. I have to pay double for my singulair (I need it to help treat my asthma) at a cvs pharmacy and I HAVE to get it in a three month supply. I was never told that they were going to make me switch to a cvs pharmacy just randomly. I had to get a three month script and they would not even give me a one month refill. Okay but then they charged me literally double for the SAME EXACT GENERIC I received at Walmart. Screw them. I’m actually considering paying without insurance at Walmart just to screw them out of that money. Okay, I can’t actually afford that but if I could then I would. Oh, and good luck getting a response from them. I’m still trying to get them to tell me why I have to get three months and why I have to get it at CVS but they just keep telling me the price and that I have to get it at CVS as a three month supply. Oh and did I mention my inhaler is $20 more through them? Luckily I haven’t had them make me switch to CVS for that too. These people are crooks. Three months at walmart is about $210 while it’s $374 at CVS. Hmm it must cost so much more to get the medication to CVS than it does to get it to Walmart.
Perhaps there s a Costco near you? You don’t have to be a member to use the pharmacy. It’s less expensive if you are, but it’s not required. Costco is good to their employees, unlike Walmart, CVS or Walgreens. It’s worth a phone call to do the price check.
To truly understand what is going on it is imperative to understand the criminal role of the PBM and their relationship to the specialty pharmacy. Pharmacy Benifits Mangers such as CareMark or Medco set the insurance reimbursements and co- pay amounts for insurance companies for expensive medication. A few years back our government allowed the largest PBMs to BUY the largest pharmacies – crazy huh. CareMark owns CVS and Medco owns Express scripts. So now the company that tells you how much a medication will cost you is the largest buyer of that med. Gee? One would think that is a conflict of interest.
I run a healthcare company that specializes in parient drug compliance and in particular RA biologic meds. I can help you with this cost issue but not sure how to reach out to you. I can put you in touch with one of our patient care advocates ( there is no cost it’s what we do all day) One of my Board Members forwarded this blog to me knowing my background.
Steve Kress
you work there
ive had cvs since 2008 i had a verry bad car accident i had to go get a mri to see what was wrong turns out i have a fracture in my back with many othere nerve problems..this is the reason im in so much pain i tried advil and every other otc meds did nothing for my pain i now see a dr every month i finally go put on a pain medication that worked very well took almost most of the pain away and i was able to get back to work and do as i did before the accident ..well the medication i was on had started to get hard to find at pharmacys so i talked to my insurance company and they told me they had a mail service and would fill my medication so i started mailing my perscriptions in and they filled it since 2009 and ive been going to the same doctor since 2009 every month now and been taking same medication ,well the last 3-4 months ive had nothing but problems with CVS CARMARK not wanting to fill my medication and this last month they canceld my order and this is not a medication you just stop taking the pain is so bad ive been bed riddin since the 20th of november i tlked to everyone possible at caremark and not one person can tell me why they wont fill it…i pay cvs caremark alot of money every month for there services im so pissed im just gana cut to the point CVS CAREMARK IS THE WORST INSURANCE COMPANY . i called and talked to the dea and fda and faxed them my medical records and prescriptions and they went threw it and called me back told me there was no reason why they will not fill my scrips … this is not right do ur job carmemark and fill prescriptions like your supose to instead of making the people that need there meds so we can have a life without pain …i wish all you pharmasits that have decided not to fill prescriptions could walk in my shoes for a month and have to deal with these problems you give me and all others with this problem and there are a lot google it and see how maney people HATE caremark 94% of people that have to use caremark Hate you only 6% like you thats bad get ur shit togeather
HI there, I’m a Medical & Orthopedic massage therapist, and I may be able to give you some helpful news. There is a special type of X-Ray, called a digital motion x-ray (DMX for short). It’s very good at finding small fractures and ligamentous instabilities that only show up when you move. A still motion x-ray won’t show them. An MRI can’t be done while moving, and a tear in a small accessory ligament on the inside of the spinal column between the vertebrae can’t be seen any other way, nut it can make your life a living hell by not “springing” the vertebrae back into position after a movement, and leaving it leaning on the nerve. Please go to You Tube and look up Digital Motion X-Ray, the videos will amaze you. They shoot at either 24 or 30 frames per second, while you’re doing the movement that hurts. I’ve been in my field 30 years, I spent 5 of it working for an orthopedic surgeon, and this is one of the most amazing things I’ve ever seen. Once you’ve done that, google “Digital Motion X-Ray” and the name of your town or nearest good sized city (200K people). Chances are, you’ll find one. There are also a fair number of veterinarians who have one, and they may know who has a human one. I hope you get the help you need, both with the cause of daily pain, and getting needed meds.
My husbands insurance company has just switched us to Caremark and I have not had time to really see how things are going to work. As far as cvs pharmacy I love them. Everytime I have gone there they go above and beyond to help if there is a problem so I don’t have a problem using cvs since that is all I have used for years. As far as Medco/express scripts I hated them. They hardly covered anything. My teenage daughter had knee issues and had been on Celebrex for sometime but when we switched to express scripts they stopped covering it. My other daughter had allergies and they stopped covering her singulair and said we had to have proof that other things had been tried for a good period of time before they would cover it. The doctor confirmed and they still denied. I do believe the health insurance company makes the rules on what they will cover and what they will not. I do not believe that caremark makes those decisions.
I had a similar experience with walgreens. I went to the walgreens to refill my prescription for acid reflex. The same pharmacy I’ve been using for years. All of a sudden, they wont take the prescription carrier. I was told we dont do business with them anymore. The medicine was only $10, because my wife who is the secondary coverage kicked in. Few months later Walgreens is now doing business with express scripts. Only problem, long term medication has to be mail order. I was never told until i tried to refill my medication. The pharmacist wouldn’t even take the secondary coverage. So I left and call my HR and they gave me the info to get the medication by mail. But it takes two weeks to get the info processed. In the mean time I’m suffering, can’t sleep, and feel bad. Last Sunday I decided to take the refill bottle to walgreens and some lady who I didn’t know, filled my prescription. I got lucky. Walgreens and CVS are cutting out the middle man, the pharmacist. I went to my union president and suggested we change prescription carriers.
I hope CVS goes out of business, or at least my benefits coordinator chooses another provider, ANY other provider!!! Just please get rid of CVS!
Since Express Scripts bought out Medco, there are only two PBM services: eScripts and CVS CM. Both are terrible. But, if CVS goes under, then there will be no competition.
Better to fight them with pen and ink. Wtite to A.G. Holder at Justice if you feel their actions rise to the level of criminal malice.
I have dealt with Caremark for all my meds for years and never had a problem. I get a 3 months supply of Enbrel via mail which is always prompt and the medication packed in ice. UPS is very dependable in delivering on the day I expect it to come. Caremark is good about calling me when it’s time to reorder before running out which is appreciated. As far as a refund for the one RX you had to pay for: I don’t see where Caremark would be expected to do that since it was United that should have informed you of the change. I applaud both CVS Caremark and UPS!!
Caremark mail-order pharmacy @#&***#%. They caused me to pay $298 for Lantus because they wouldn’t send our prescriptions. I talked to The Goodyear Dunlop Benefits person and she said do not even use the mailorder pharmacy since we had so much trouble with them. Just to have them transfer the prescriptions to CVS in our town. They only transferred 3 of 5 and said they would mail the other 2 to us. A week later we were nearly out of synthroid and the prescription had not been mailed. Now mind you we had told them we did not intend to us their service and to transfer the prescriptions to CVS locally. I then got an e-mail that they had just received a new prescription and they were processing it. They didn’t get a new prescription. They were processing one that they were told to transfer. They had had it over a month. They not only processed and shipped it but they charged it on a debit card they had already been told not to use. Even though they had another debit card number to use. ( they were told to delete the improper card out of the system) I had to cancel the card to stop their payment and fill out all sorts of papers at the bank protesting the charges they had put through. I received the meds and because the novolog included in the order is perishable and must be refrigerated I opened the box and will have to pay for the shipment. I was afraid I would end up having to pay full price upfront for the insulin again If I didn’t keep this. They are charging an unreasonable co pay for the synthroid and insulin and only sending 1 months supply. If I have to pay copay every month, I will not use CVS, even the local. We have a great mom and pop and I will use them. Oh by the way. To even finaly get to this point, I have spent at least 25 hours in 1 month dealing with “CVS (don’t) caremark mailorder Pharmacy ,customer (don’t) care.” They have given more than 5 different reasons for not sending my husbands medicines that are essential to his life. One sweet lady did get me a refund for the Lantus that I had to pay for. After 4 weeks of fighting with them for our meds, They told me they couldn’t deal with me because I wasn’t the member. If they had told me that up front I would have mailed my legal paperwork to them stating that I am required by the courts to take care of my husbands financial, medical, and legal affairs. Since so much time had elapsed, I was tired of messing with such a messed up business. They are typical for anything connected with the government. The older people of our nation are just dirt under their feet and they would just prefer for us to die.
no fan of un Caremark or CVS
True. They are just suppliers. And, it is the patients responsibility to read and understand changes in their health insurance policy.
RN Minnesota: I am at the point of choosing a Medicare Advantage Plan or Part D stand alone and cannot find out what the contracted cost of Orentia (abatacept) is for each plan. BC/BS said it is not covered and my cost would be $10,000 per month or $131,000 per year. Others say a prior auth could be described because I have been on all other injectables and RA oral meds. Orencia is the first one to work and now the co-pay assist from Orencia goes away because Medicare is a government program!!!! How does that change anything in the cost to me? Please let me know if any of you have found a Medicare Part D that covers Orencia with a reasonable copay. UCAre was going to be 25% of ______ what cost ? $3,000 or $800 copay? CVS has delivered my drugs as requested when needed. They just do not help with insurances decisions or information on costs for Medicare. Should I go to out-patient is the other question? Has that been covered for any of you?
“…and cannot find out what the contracted cost of Orentia (abatacept) is for each plan.” And they won’t tell you, either. Both the Plan Sponsor and the Insurer usually receive a percentage of rebates and discounts provided by the drug manufacturers. The most you can usually weasel out of the PBMs is the cost calculation based on something they refer to as the Average Wholesale Price (AWP). The AWP is sort of like BigPharma’s equivalent of an auto dealer’s manufacturer’s suggested retail price on the stickers for new cars. Needless to say, it made little sense even to The Spouse, who has a Ph.D. in Number Theory. ALSO, a Prior Authorization form may not be enough for some drugs. If CVS/Caremark is your PBM, they often require a Brand Penalty Exception form be filed for brand name pharmaceuticals for which generics or therapeutic equivalents are available. This requires more detailed medical information than your usual Prior Authorization form. Consequently, many specialists will not fill them out if you FAX them in. Request the form and schedule a physician visit soon, to plan for the 2015 Plan year.
I am a juvenile diabetic & had not one issue with MEDCO!! I recently was switched to cvs caremark & am running into same problems!!! They are the absolute worst!!! I paid $798 out of pocket today for my sanity and well-being!! God forbid if your doctor writes “name brand medically necessary” on your rx…. Forget bout it… They box you in bc they conveniently dont carry it in stock & yet if you go to any other local pharmacy, you have to pay out of pocket!!! That alone should be illegal since they are a pharmacy NOT A DOCTOR!!! When i contacted my employer, they were angry & tried to go to bat for me as well on these issues, yet nothing has changed … Im still paying $798 month!!! I give them a Grade F bc i have insurance yet im paying full price on meds!!!
That’s a nightmare, I’m so sorry. I finally got mine worked out but it involved shipping it to my neighborhood CVS where I then pick it up from a store manager. The time they forgot to refrigerate it and had to eat the $6,000 cost compelled them to allow me to get it from a pharmacist rather than a store manager.
I’m glad it was their money and not mine. Hopefully your employer can be helpful. I called ours teary and they were able to affect some change.
I’m in the same boat with CVS Caremark. My son has MS so his medicine must be shipped by a specialty pharmacy – we were using Walgreens & everything was GREAT then our insurance forced us to switch to CVS Caremark & it’s been constant problems. Every refill is a fight – not the day I call in the refill but days later right before it is supposed to ship then it’s a weeks worth of phone calls just to get medicine shipped right on time for his weekly shot.
UGGGGGGHHHHH that sucks in every possible way. I have mine mostly worked out but I feel anxious every time I call them like I’m hoping it will actually be okay.
Please file a complaint with your state’s insurance commissioner. When the government starts looking at business practices, companies often start acting more reasonable.
CVS Caremark is THE WORST. My current order of Enbrel has been in transit for 3 days already and I have been like a prisoner in my house waiting for it. My insurance (United) changed me to Caremark from a previous mail order pharmacy. The previous mail order pharmacy was a pleasure to work with – prompt, deliveries on time, refills painless and they contacted the doctors timely when prescriptions ran out. Caremark has been nothing but a nightmare from day one. Hundreds of phone calls just to transfer my two prescriptions in the beginning and every month several time consuming calls to get the prescription and because the deliveries of (supposed to be refrigerated) medications are not timely. Just getting through the phone tree and looking up my information takes about 5 times as long as it did with the previous pharmacy – their phone operators don’t even seem to know the names of the letters of the alphabet, so trying to get them to get my last name right, for several calls each month, is PAINFUL.
Now I have them ship it to the local CVS. I don’t need $6k worth of medicine sitting on my front porch heating up in the sun.
Having very similar issues with CVS Caremark and would greatly appreciate any ideas. I do not think this crazy and immoral behavior should be allowed to continue without being addressed. They also insist on special “rules” when getting prescriptions at a pharmacy other than CVS, even though their own pharmacies are often unable to get certain medications. Should we not go after them together?
You should READ and learn your insurance coverage. The emails and paperwork they send you in the mail are very informative. Know and understand what is covered through your insurance agreement that is YOUR responsibility. All insurance cards have a member services phone number on the back and websites to go and seek information.
I have SILVERSCRIPT and I called them. They cover the medication CVS suddenly refused to fill. THEY even called CVS to ask them why they are denying filling it. Your response is wrong on this issue. CVS makes up their own random rules based on the weather or if they got laid the night before or not.
We started using Caremark/CVS on January 1, 2015. Since I was in the hospital and rehab, I took the meds in those places. The rehab place sent the remainder home with me since I had paid for them. I finally needed a very important pain pill in March. I sent in the hard copy expecting the same service I have had for ten years at several different mail order pharmacies. I was told by letter that the generic was not on my formulary, but they owed me one 30 day supply legally to give me time for an appeal or to find other meds to take. The next I knew they did not have the pills from the supplier. I asked them to supply with the brand name. They kept finding one excuse after another, but did not fill the prescription. After two weeks, I was out of the meds I had. They did not seems to care. One of their pharmacists told me to take over the counter meds or go to the emergency room. If she really was a pharmacist wouldn’t she know that over the counter meds would not help after ten years of very strong pain meds? The following Monday I got on the phone with an insurance rep to help me. They told us that now we were past the 90 days since we joined Caremark, and they did not have to supply me the one time fill. It certainly was not my fault that the 90 days was over. They were the ones not filling the prescription. I was the one in withdrawal. To make a long story short, my doctor, who was very upset by Caremark, wrote a new prescription, I went to pick it up, and Walgreens filled the prescription with the brand name. But, the first prescription remained in process. I asked to cancel it, and was told by a very impolite person at their care center, that it was my fault and it would not be filled anyhow because now there was a quantity limit. I said to please cancel the order. I had my pills and would not pay out of pocket for another prescription. She finally canceled the order, but now that the QL has been approved I hope they do not fill it and charge me full price. I talked to two service reps who were kind, Peggy and Debbie. Otherwise, I was treated like I was not worth anything.
Cvs Caremark is the worst greedy unsympathetic people. You can get a trained monkey to do what they do. Supposily the computer went down and lost my records. Sure it did! They approve you for the cheapest medication but the expensive medication won’t be paid for. I am going to put a hippa request and see what comes. You know with the economy the CEO has to make 32 million a year while people are dying. Now of them have a brain to even think. Everything to them is denied. I hope he gets really sick and they refuse his medication.
Unfortunately all of the comments here have zero impact on the way Caremark manages their customers prescriptions. They have NO RIGHT to just change my quantity and duration of days that I can fill when the provider didn’t change, nor did my medication. Is CAREMARK a Doctor now? I thought they were the insurance provider! CAREMARK is GARBAGE.
Unfortunately I’ve had similar experiences with CVS Caremark through previous employers. My husband started a new job and when we learned CVS Caremark provided the prescription coverage I immediately advised my husband to work there a year and leave. Now our monthly prescription cost now exceeds what we pay for 3 children to attend a private high school. CVS Caremark has crippled our finances.
Unfortunately I’ve had similar experiences with CVS Caremark through previous employers. My husband started a new job and when we learned CVS Caremark provided the prescription coverage I immediately advised my husband to work there a year and leave. Now our monthly prescription cost now exceeds what we pay for 3 children to attend a private high school. CVS Caremark has crippled our finances.